For years, the idea of undergoing a heart surgery has evoked unfathomable fear and apprehension in patients. This is primarily because of the anxiety of “cracking open the chest” – the what-ifs associated with such a ‘complex surgery’. The mere thought of cutting the breast bone with a saw is not just mentally traumatic but gives rise to crippling fear, anxiety and apprehension.
The matter of fact is, that all these fears are not unjustified.
It is a reality that sternotomies (cutting open the breast bone), do result in profound post-operative pain. This pain often discourages the patient from taking adequate breaths, resulting in delayed weaning from the ventilator. Even post weaning, patients, commonly exhibit shallow breathing, which again results in collapsed lungs and oxygenation issues. This automatically slows down the recovery process requiring late mobilization and prolonged hospital stays. Increased blood loss either during surgery or due to injury while closing the sternum is another point of worry. This may require increased blood transfusions or even re explorations in case of persistent bleeding.
The vulnerability of the sternum, necessitates a longer recovery and rehabilitation of around 3 months. During this period, if proper care is not taken, wound infection and sternal dehiscence too may occur. This essentially means that the sternum may fail to fuse and give way. This is an extremely worrisome complication which increases morbidity manifold, especially in diabetic, obese patients.
All the above reasons often deter patients from opting for cardiac surgery. They often end up choosing stents for even scenarios where bypass (CABG) would normally be indicated.
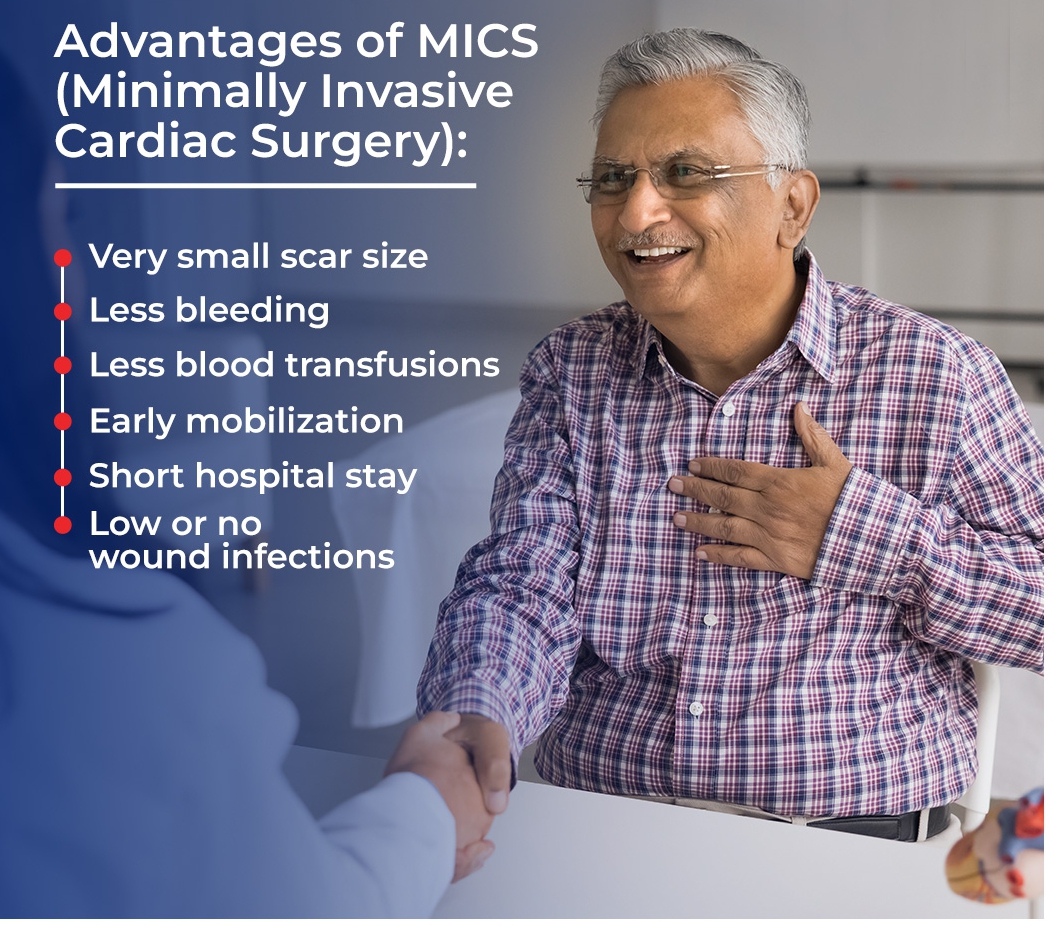
This is majorly due to lack of awareness and availability of MICS, i.e., Minimally Invasive Cardiac Surgery. This essentially means that the same cardiac surgery can be done without a midline sternotomy. The entire procedure is done by a small incision, between the ribs. This could be either on the left or right side, depending on the procedure.
The most common procedures that are done by this method include MICS CABG or Minimally Invasive Direct Coronary Artery Bypass Grafting (MIDCAB), MICS Valve Replacements (Mitral/Aortic or both), MICS Atrial Septal Closures and Tumour (myxoma) removals.
In cases of valve replacements or ASD closures, where the patient will require a cardiopulmonary bypass to redirect circulation, groin cannulation is performed instead of the conventional open method.
This not only drastically reduces the scar size but also ensures fewer blood transfusions, early mobilization, and short hospital stays. Wound infections are much less likely and chances of sternal dehiscence is completely avoided.
The rehabilitation period is shortened to less than a week as compared to 3 months, which is an absolute game changer.
Any difficulties faced in MICS are more for the surgeon than the patient, as it requires immaculate skill to perform the same surgery through a smaller incision. This may result in a slightly longer operating time. Another limiting factor could be the disease itself, like an extensive right coronary artery disease may not be well accessed through a left sided MIDCAB incision.
However, the benefits of this procedure out-weighs its limitation by miles. There is no difference in long-term prognosis of MICS when compared to the conventional approach, hence it is slowly becoming the order of the day.
At Peerless Hospital, Kolkata, we have acquired all the necessary equipment for performing these cutting-edge procedures. We perform MIDCAB (Minimally Invasive Direct Coronary Artery Bypass) procedures regularly with fantastic results.
Our patients go home in 3 days with minimal or no blood transfusions and minimum post-operative pain. On follow-up good progress is seen in recovery with hardly visible scars.
So, if someone is putting off heart surgery out of fear, they should know that the era of Minimally Invasive Cardiac Surgery is here — and it is transforming lives with smaller scars and bigger wins.
Senior Consultant, Cardiothoracic & Vascular Surgery, Peerless Hospital